 Actuality of the problem. General practitioners, neurologists, cardiologists, therapists in their daily practice often face a headache problem. Among the primary headaches, a special place is given to one of the most common vascular headaches – migraine, which affects up to 12% of the world’s population. The disease has a well-defined hereditary nature (the risk of illness in children with a hereditary burden on the mother’s line is 72%, along the line of the father – 30%, with migraine in both parents it reaches 80-90%) [2, 5, 6, 13]. The prevalence of migraine and its negative impact on the quality of life cause a great urgency of the problem. Migraine is a chronic neurological disease that differs in frequency of periods of exacerbations, severity of the course, and influence on patients’ quality of life [4, 8, 9].
Actuality of the problem. General practitioners, neurologists, cardiologists, therapists in their daily practice often face a headache problem. Among the primary headaches, a special place is given to one of the most common vascular headaches – migraine, which affects up to 12% of the world’s population. The disease has a well-defined hereditary nature (the risk of illness in children with a hereditary burden on the mother’s line is 72%, along the line of the father – 30%, with migraine in both parents it reaches 80-90%) [2, 5, 6, 13]. The prevalence of migraine and its negative impact on the quality of life cause a great urgency of the problem. Migraine is a chronic neurological disease that differs in frequency of periods of exacerbations, severity of the course, and influence on patients’ quality of life [4, 8, 9].
When drawing up a treatment plan, it is necessary to take into account not only the diagnosis, symptoms, the presence of certain concomitant diseases, but also the patient’s expectations, needs and goals. The patient, when talking to the doctor, he is waiting for relief and relief of pain, and in the future hopes for a complete cure for his disease.
The feeling of expectation of a headache with migraine leads to emotional instability, capriciousness, down to the development of depression, which is fraught with the development of psychological maladaptation of patients [1, 7, 10]. This explains the efforts of modern medicine to find ways of preventive, curative and rehabilitative therapy with one or another nosological unit.
According to the American Migraine Prevalence and Prevention (AMPP), 38.8% of patients with migraine require a preventive approach. Of these, 13.1% of patients need to consider the need and the possibility of prescribing preventive treatment, and 25.7% of patients need preventive treatment for migraine. Unfortunately, only 13% of all migraine patients are currently taking preventive therapy [1, 11, 13, 14]. For some patients, the problem of headache is not particularly significant, although they suffer for years, up to the development of complications, and therefore the number of patients with headaches, in particular migraine, remains statistically significant [12, 18, 20, 23].
The problem of migraine is actual and in connection with the difficulties of diagnosis and treatment of this pathology. Migraine is not a life-threatening disease, but it significantly reduces the quality of life of patients. The World Health Organization migraine is included in the list of 19 chronic diseases, the most violating the social adaptation of patients [15, 18, 20, 22]. Patients with migraine suffer for years, try out existing traditional analgesic drugs, despite their side effects, but do not get the expected effect, which leads to depression, emotional instability, violation of physiological biorhythms: sleep-awakening, a desire to rejoice, communicate with Relatives, doing ordinary daily work, the interest in one’s own existence as an individual disappears [7, 15, 17, 21, 24].
Moreover, the treatment of patients with chronic migraine and migraine status often puts before the fact the absence of effective drugs at hand with a persistent and rapid therapeutic effect. The duration of the course and severity of headaches with migraine leads to the development of depression is twice as high as in people without migraine attacks [3, 19, 25]. Researchers (University of Toronto) found that among men, depression with migraine headaches reaches 8.4%, while among women it is 12.4%. Women suffering from migraine are more prone to emotional changes and depressive mood [26, 27]. According to the US data for 2013 migraine significantly increases the risk of depression in women, as evidenced by a survey of 36,000 respondents.
As the analysis of the data showed, women who had migraines, 36% more often complained of depression. Patients who suffered migraine with aura suffered from emotional problems 43% more often than women who never experienced migraines. Headaches without an aura increase the risk of depression by 29% [28, 29, 16]. In connection with the analysis of the data given, it became interesting for us to conduct our own study of the data of the psychological status depending on the severity of pain associated with migraine.
Thus, the purpose of this study was to examine the psychological status of patients with complicated migraine depending on the intensity and duration of headaches.
Material and Methods: We examined 106 patients (100%) between the ages of 26 to 46 years (mean age 36 ± 2,8 years). Patients are divided into 3 groups, 38 (40.3%) patients with migraine associated with migraine status 1-group, 46 (48.8%) patients with chronic migraine 2-group, 22 (23.3%) patients with migraine Associated with migraine stroke 3-group. An analysis was made of clinical-neurological data, of psychological status studies using The Hamilton scale for assessing depression (HDRS-21). An analysis of the nature and intensity of pain was carried out using one-dimensional intensity scales – the numeric rating scale (NRS), the verbal rating scale (VRS) and the visual analog scale (VAS)
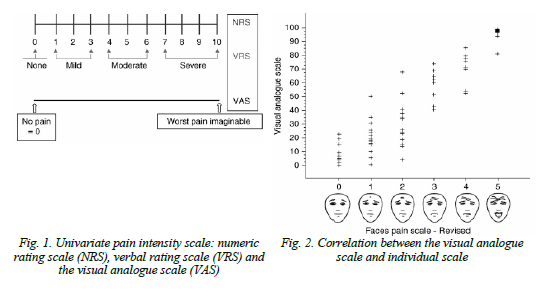
The “absence of pain” on the VRS scale was 0 on the NRS scale, “minor headache” was noted 1-3 in a linear gradation, “moderate headache” 4-6, whereas on the VAS scale these were marked as “absence of headaches Pain, 7-10 linear gradation on the NRS scale was noted as “severe headaches” on the VRS scale and as “worst headaches” on the VAS scale. The VAS data were compared with facial pain scales (faces pane scale).
In the study of the psychological status according to the scale of Hamilton (HDRS-21), the examination with each patient took 20-22 minutes. The evaluation time was defined as “during the last week”. The value of scores for nine items was designated as – from 0 to 4. Six points in which the symptoms could not be expressed quantitatively were evaluated qualitatively – from 0 to 2.
The sum of the scores from the evaluation of persons who did not suffer from depression, with complicated forms of migraine, was estimated as 7-16 points. In patients who deviated from the answers, their relatives were connected, while direct questions were minimized. Repeated studies on the Hamilton scale after treatment were performed and evaluated without previous preview of the previous measurement, on a clean record sheet.
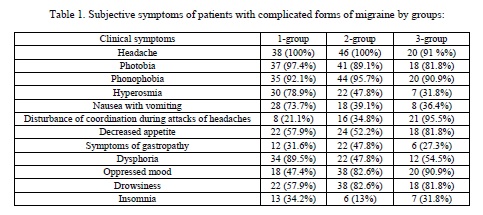
Results and discussion of the study. In the analysis of clinical and neurological changes, the following data were revealed: headaches of a paroxysmal nature pulsating by the type of hemicrania were noted in 32 (84.2%) patients 1 g, 32 (69.6%) patients 2 g, 9 (41% ) Patients 3 g. Two-sided headaches were noted in 4 (10.5%) patients 1 g., 5 (10.9%) patients 2 g., 10 (45.5%) patients 3 g. Pains of a paroxysmal nature in the nape of the nape were noted in 2 (5.3%) patients 1 g., 5 (10.9%) patients 2 g., 1 (4.6%) patients 3 g. Heaviness in the head was noted in 2 (9.1%) patients of the 3rd group. Migraine attacks were often accompanied by photophobia in 37 (97.4%) patients 1 g., 41 (89.1%) patients 2 g., 18 (81.8%) patients 3 g. Phonophobia and hyperacosta during the attack suffered 35 (92.1%) patients 1 g., 44 (95.7%) patients 2 g., 20 (90.9%) patients 3 g., Hyperosmia suffered 30 (78.9 %) Patients 1 g., 22 (47.8%) patients 2 g., 7 (31.8%) patients 3 g., Nausea, sometimes accompanied by vomiting, suffered 28 (73.7%) patients 1 g., 18 (39.1%) patients 2 g, 8 (36.4%) patients 3 g, loss of spatial orientation and dizziness suffered 8 (21.1%) patients 1 g, 16 (34.8%) patients 2 Gr., 21 (95.5%) patients with 3 g. Often there was a delay in the stool, a feeling of overfilling and overeating in 12 (31.6%) patients 1 g., 22 (47.8%) patients 2 g., 6 (27.3%) patients 3 g., Refusal of food And a decrease in appetite was observed in 22 (57.9%) patients 1 g., 24 (52.2%) patients 2 g., 18 (81.8%) patients 3 g. Irritability (dysphoria) for any reason was noted in 34 (89.5%) patients 1 g., 22 (47.8%) patients 2 g., 12 (54.5%) patients 3 g. Oppressed, depressed mood with general lethargy was observed in 18 (47.4%) patients 1 g., 38 (82.6%) patients 2 g., 20 (90.9%) patients 3 g. Drowsiness tormented 22 (57.9%) patients 1 gr. After painful attacks of headaches, 38 (82.6%) patients 2 g., Regardless of the attacks of headaches, 18 (81.8%) patients 3 g. Permanent character (this symptom is subject to careful analysis in further studies). Insomnia suffered 13 (34.2%) patients 1 g., 6 (13%) patients 2 g., 7 (31.8%) patients 3 g. Table 2 shows the data of subjective sensations for the groups under study.
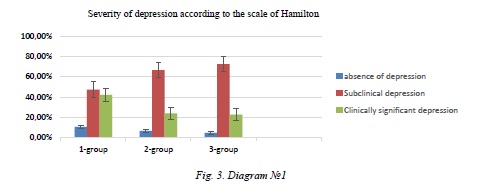
According to the Hamilton scale (HDRS- 21), the absence of symptoms was significantly expressed (from 7 to 16 points), anxiety and depression were detected in a small amount of patients with complicated forms of migraine, respectively, in 4 (10.5%) of patients with 1 gr., 3 (6 , 5%) of patients 2 g., 1 (4.6%) of the patient 3 g. Subclinical depression (from 17 to 27 points on the Hamilton scale) was detected 20% more o ften with chronic migraine than in patients with migraine status, and 40% more often than with migraine strokes, as it looked in patients with complicated migraine forms As follows: 18 (47.4%) patients 1 g., 32 (66.7%) patients 2 g., 5 (22.7%) patients 3 g. Clinically significant depression (more than27 points) was detected 20% more often in patients with migraine status than in patients with chronic migraine, and with migraine stroke it was 40% more frequent than with chronic migraine, respectively, this figure looked like this: in 16 (42.1%) patients 1 g., 11 (23.9%) patients 2 g., 16 (72.7%) patients 3 g.
Diagram 1 shows the severity of depression on the Hamilton scale by groups.
One-dimensional pain intensity scales showed a slight headache (according to VRS, which is equal to NRS from 1 to 3 linear gradations and there is no pain on the VAS scale, and compared to the facial scale (FPS) it was equal to 1-2 points) in 3 (7.9%) patients 1 g., 13 (28.3%) patients 2 g., 6 (48.3%) patients 3 g., The severity of depression in these patients was assessed as the absence of depression in all 3 (7,9%) patients 1 g, in 2 (5,3%) patients 2 groups, and in 1 (4,5%) patients 3 g, subclinical stage of depression was observed in 10 (26,3%) patients 2 g., In all 5 (22.7%) patients of the 3rd group, clinically significant depression was detected in 1 (2.17%) of the patient with 2 g;
Moderate headache (according to the VRS scale from 4 to 6 linear gradation according to NRS, absence of pain according to VAS, and in comparison with the facial scale (FRS) is 3 points) was revealed in 8 (21.1%) patients 1 g. , 21 (45.7%) of patients in 2 groups, 12 (54.6%) of patients with 3 g, with 1 depression (2.6%) in 1 patient, 1 (2.2%) in 1 2 groups, subclinical stage of depression was observed in 8 (21.1%) patients 1 g., 14 (30.4%) patients 2-g., 3 (13.6%) patients 3 g., Clinically expressed depression was detected in 6 (15.8%) patients 1 g., 4 (8.7%) patients 2 g., 5 (27.7%) patients 3 g.
Severe headaches (according to the VRS scale, 7-10 linear gradations in the NRS, and 7-10 scales on the VAS scale, and with a comparison with the facial scales of 4-5 points) were observed in 27 (71.1%) patients 1 g. , 14 (30.4%) patients 2 g., 2 (9.1%) patients 3 g., While subclinical stage of depression was observed in 10 (26.3%) patients 1 g., In 22 (47.8 %) Patients 2-g., 3 (13,6%) patients 3 g. Clinically pronounced depression was noted in 10 (26.3%) patients 1 g., 6 (13.1%) patients 2 g., 11 (50%) patients 3 g.
Summing up the results of clinical observation of the development of the pathology of the psychological status of patients with complicated migraine forms, one can determine the effect of pain syndrome, and in particular the headache, on the degree of development of depression. Headache can be the cause of the development and aggravation of the symptoms of depression and the development of social maladaptation in patients with complicated forms of migraine both because of the actual headache and apparently, and because of the development of pathobiochemical mechanisms of the destruction of the substance of the brain itself.
As can be seen from the data presented in the clinical experience, with migrenosal status, subclinical and clinically severe depression is seen in severe headaches, with prevalence of subclinical depression with moderate headache, which is apparently associated with the duration of headaches and short periods of remission.
With migraine strokes, the frequent occurrence of clinically pronounced depression is associated with focal lesions and abnormalities in the patho- chemical mechanisms of brain activity. The existing depression can aggravate the intensity of the pain syndrome and its duration, leading to a reduction in the periods of remission, developing a continuous chick pain-depression-pain.
Conclusions: Thus, the development of the pathology of the psychological status, and in particular depression in patients with complicated forms of migraine, leading to social exclusion of patients exacerbates the complicated forms of migraine, enhances the intensity of headaches, prolonging the time of their existence, and requires timely correction and preventive treatment of this disease . And by the reverse chain – the intensity and prolonged existence of headaches and short periods of remission between them can lead to the development of deep depressions down to the decline or lack of efficiency of persons of working age. In this regard, it is necessary to develop ways of preventive and rehabilitation therapy of the pathology of psychological status in case of migraine to break the chain of pain-depression-pain.
REFERENCES
1. Amelin A.V. Prevention of migraineous paroxysms / / New technologies in the diagnosis, treatment and rehabilitation of neurological diseases. – St. Petersburg., 2010.
2. Batysheva T. T., Kostenko E. V., Ganjula P. A. The complex program of secondary prevention of stroke: the place of the drug Vazobral. Cons. Med. 2007; 9.
3. Grigorieva V. N., Gustov A. V., Kornilova L. E., Kulikova O. A. Efficiency of the combined use of kinesitherapy and psychotherapy in the treatment of migraine patients // Zhurn.Neuropathol. And a psychiatrist. them. S. S. Korsakov. – 2003. – T. 103 (12). – S. 20-25.
4. The international classification of headache: Translation V. V. Osipova, T. Ascension. – Edition 2. – 2003. – 219 p.
5. Mishchenko T. S., V. N. Mishchenko Current diagnosis and treatment of neurological diseases // Directory doctor “Neurologist”. – LLC “Doctor Media”, 2010. – P. 65-74.
6. Mozolevski U. V., O. V. Assumption, Cherkashin A. V. Migraine stroke. Pain 2006; 4 (13): 25-30.
7. Morozova O. G. Migraine: Questions comorbidity and differential diagnosis // Health Protection of Ukraine. – 2010. – № 4. – S. 19-20.
8. Morozova O. G. Migraine: problems of classification, diagnosis and treatment // Health Protection of Ukraine. – 2010. – № 4. – S. 17-18.
9. Handbook of Headache / Kadykov AS, Shahparonova NV Manvel LS – M .: “Milkosh”, 2005. – 170 p.
10. Suchasna dіagnostika i have lіkuvannya nevrologії that psihіatrії / For Ed. TS Mіschenko, VS Pіdkoritova. – K .: TOV “Doctor Medіa”. – 2008. – 624 p.
11. Tabeeva G. R. Migraine Prevention. Manual M .: Pulse 2008.
12. Stem V. N. Headache. – M: “Medinformagenstvo” Ltd., 2007. – 472 p.
13. Yahno N. N., Parfenov V. A., Alekseev V. V. Headache in cerebrovascular diseases. In: Headache. Moscow, 2000: 73-8.
14. Arboix A, Massons J, Oliveres M. Headache in acute cerebrovascular disease: a prospective clinical studying 240 patients. Cephalagia. 1994; 14: 37-40.
15. American Academy of Neurology: Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for prevention of migraine. Accessed online November 8, 2005.
16. Boska M. D., Welch KMA, Bar -ker PB et al. Contrasts in cortical magnesium, phospholipid and energy metabolism between migraine syndromes // Neuro- logy. – 2002. – V. 58. – P. 1227-1233.
17. Charles A., Brennan K. C. Cortical spreading depression – new insights and persistent questions // Cephalalgia. – 2009. – V. 29. – P. 1115-1124.
18. Connor K. M., Shapiro R. E., Diener H. C. et al. Randomized, controlled trial of telcagepant for the acute tretment of migraine // Neurology. – 2009 – 22 – 970-977.
19. Gasbarri A., Armone B., Pompili A. et al. Emotional memory and migraine: Effects of amitriptyline and sex related difference // Behav. Brain. Res. – 2008. – 189 – 220-225.
20. Goadsby P. J., Lipton R. B., Ferrari MD Migraine – current understanding and treatment // New Engl. J. Med. – 2002. – 346 – 257-70.
21. Goadsby PJ Migraine, aura, and cortical spreading depression: why are we still talking about it? // Ann. Neurol. – 2001 – 49 – 4-6.
22. Kruit M. C., van Buchem M. A., Hofman P. A. Migraine as a risk factor for subclinical brain lesions. JAMA 2004; 291: 427-34.
23. Kurth T, Slomke MA, Kase CS. Migraine, headache and the risk of stroke in women: a prospective study. Neurology 2005; 64: 1020-6.
24. Olesen J., Lipton RB Migraine classification and diagnosis. International Headache Society criteria // Neurology. – 1994. – 44 (Suppl 4.). – 6-10.
25. Solomon S. Migraine diagnosis and clinical symptomatology // Headache. – 1994. – 34. – S8-12.
26. Stang PE, Carson AP, Rose KM. Headache, cerebrovascular symptoms and stroke: the Atherosclerosis Risk in Communities Study. Neurology 2005; 64: 1573-7.
27. Swartz RH, Kern RZ. Migraine is associated with magnetic resonance imaging white matter abnormalities: a meta-analysis. Arch Neurol 2004; 61: 13668.
28. Scher AI, Terwindt GM, Picavet HSJ. Cardiovascular risk factors and migraine. Neurology 2005; 64: 614-20.
29. Welch KMA, BousserMG, Bogouslavsky J. Migrainous infarction and migraine triggered epilepsy. In: Olesen J, Goads-by PJ, Ramadan NM (eds). The Headaches. 3 d ed. Lippincott Williams & Wilkins, 2006: 599-612.
Created by Sanoyeva Matlyuba Jahonkulovna, Saidvaliyev Farrug Saidakramovich
